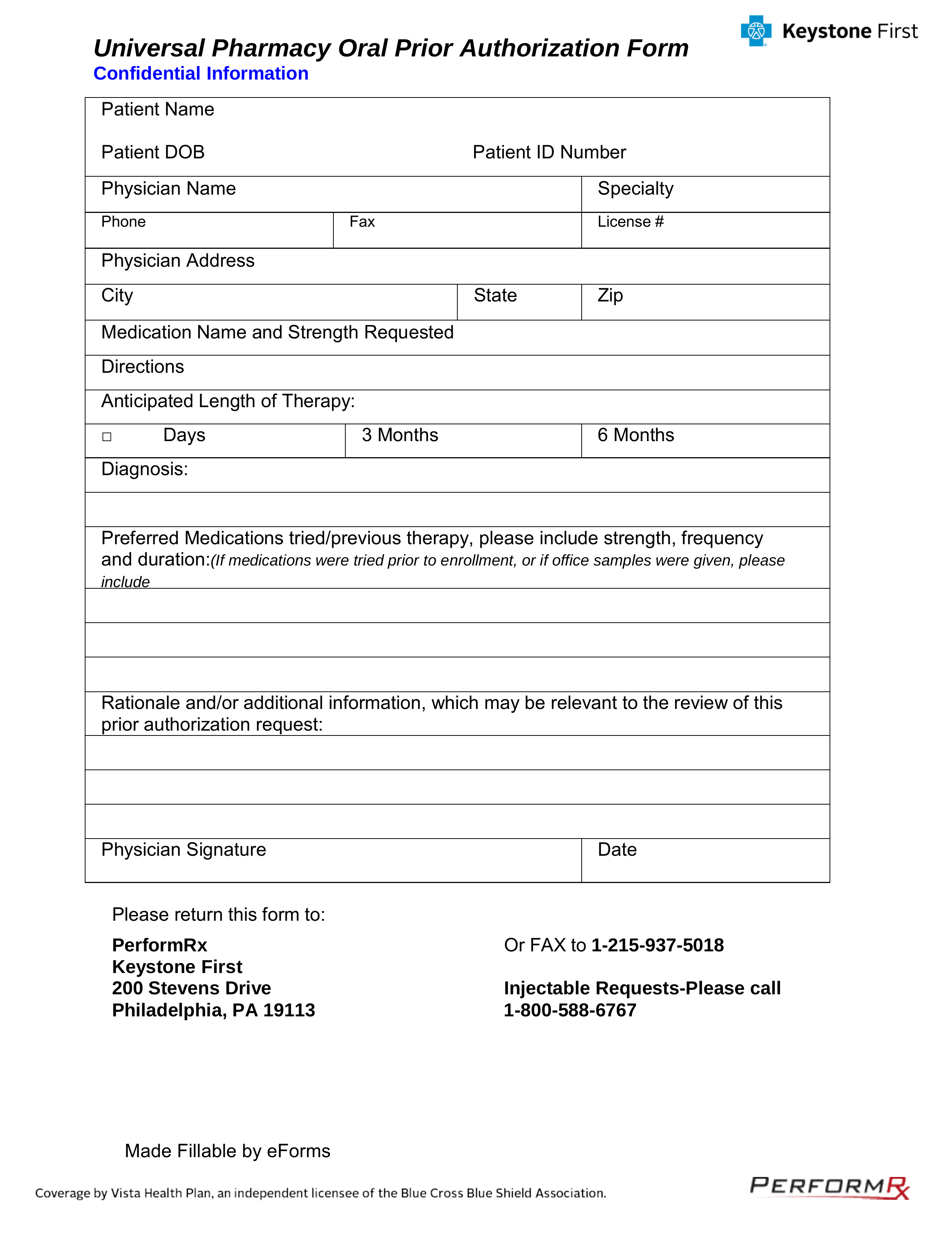
Keystone Mercy Health Plan Prior Authorization Form
Related to keystone mercy health plan prior auth keystone first authorization UNIVERSAL PHARMACY ORAL PRIOR AUTHORIZATION FORM form effective 72120Fax to PerformRxSM at 12159375018 or to speak to a representative call 18005886767. For more information on the pharmacy prior authorization process call the Pharmacy Services department at 1-866-610-2774.
Free Keystone First Rx Prior Authorization Form Pdf Eforms
You pick a primary care physician PCP or family doctor to coordinate your care.
Keystone mercy health plan prior authorization form. Submit by fax using the forms posted at FutureScripts. Monday-Friday 8 am-430 pm. Non-participating provider emergency services payment guidance PDF Opens a new window.
The online prior authorization submission tutorial guides you through every step of the process. 203 Community Resources Contact Information Table. Opioid-related prior authorization request forms.
A request form must be completed for all medications requiring prior authorization. Prior Authorization Form PA form prior auth form Created Date. Keystone Mercy Health Plan produces selected ret-rospective review reports for clinical analysis and.
Please provide as much relevant medication information as possible to increase the accuracy of your submission. Always check plan benefits first. Long-acting opioid prior authorization form PDF Short-acting opioid prior authorization form PDF.
When checking whether a service requires an authorization under Mercy Cares Online Prior Authorization Search Tool please keep in mind that a listed service does not guarantee that the service is covered under the plans benefits. Outside of normal business hours call Member Services at 1-800-521-6860. MERCY CARE PROVIDER MANUAL TABLE OF CONTENTS.
Please fax completed forms to FutureScripts at 1-888-671-5285 for. Your PCP will treat you for general health needs and refer you to specialists as needed. For Participants Participants homepage View your benefits Participant handbook Find a Doctor Medicine or Pharmacy.
Keystone First coverage by Vista Health Plan an independent licensee of the Blue Cross and Blue Shield Association serving the health insurance needs of Philadelphia and southeastern. 202 Health Plan Authorization Services Table. You can fax your authorization request to 1-800-217-9345.
Your agent is the person who will make decisions about your health care if you cannot. Prior Authorization and Coordination of Benefits. Customer Service Hours of Operation.
Your PCP or other health care provider must give Keystone First information to show that the service or medication is medically necessary. Get started at our online prior authorization request form or learn more in our tutorial. The plan reserves the right to adjust any payment made following a review of medical record and determination of medical necessity of services provided.
Pharmacy prior authorizations are required for pharmaceuticals that are not in the formulary not normally covered or which have been indicated as requiring prior authorization. 1618 Prior Authorization Contacts. 2020 Keystone First Provider Manual updates PDF Opens a new window.
Prior Authorization Form Keywords. Discharge planning guide PDF Opens a. Prior authorization is not a guarantee of payment for the service s authorized.
Request form instructions Providers. Provider Manual and Forms. All requested data must be provided.
If you are interested in having a registered nurse Health Coach work with your Pennsylvania patients please complete a physician referral form or contact us at 1-800-313-8628. Call the Pharmacy Services department at 1-800-588-6767. Provider Credentialing and Contracting for all Plans.
Certain self-injectable products require an authori-zation from Keystone Mercy prior to dispensing. Incomplete forms will not be processed. Fax completed prior authorization request form t800-854-7614 or submit Electronic Prior Authorization through CoverMyMeds or SureScripts.
Monday-Friday 8 am-5 pm. Keystone Mercy Prior Authorization Form. Please click on the link below for the applicable Prior.
Incomplete forms or forms without the chart notes will be returned. Keystone First nurses review the medical information. Download the 2020 Provider Manual PDF Opens a new window.
When completing a prior authorization form all requested information on the form must be supplied. With a Keystone HMO plan from Independence Blue Cross you can see any doctor or visit any hospital in the Keystone Health Plan East network. Download a Pre-Hospital Medical Care Directive Form.
Any additional questions regarding prior authorization requests may be addressed by calling 1-800-521-6622. A request form must be completed for all medications that require prior authorization. The nurses use clinical guidelines approved by the Department of Human Services to see if the service or medication is.
Please see available prior authorization request forms below. Business Hours of Operation. For both a Living Will and a Medical Power of Attorney you must choose someone to be your agent.
Keystone First Community HealthChoices CHC is a managed care organization. Prior Authorization Form - Providers - Keystone First Author. Table of Contents Page 1 of 17.
You can also call 1.
Https Keystonefirstchc Com Pdf Providers Universal Pharmacy Pa Fax Form Pdf

Keystone Mercy Health Plan Prior Authorization Form Beautiful Nys Medicaid Managed Care Pharmacy Benefit Information Models Form Ideas

2020 Keystone First Universal Pharmacy Oral Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Https Www Keystonefirstpa Com Pdf Pharmacy Hcpcs Authorization Form Pdf
2020 Keystone First Universal Pharmacy Oral Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Https Keystonefirstchc Com Pdf Providers Pharmacy Hcpcs Authorization Form Pdf
Post a Comment for "Keystone Mercy Health Plan Prior Authorization Form"